Enhancing Psychospiritual Well-being in Patients with Progressive Neurological Diseases
Lily Chan Man-lee | Year 3 Doctor of Philosophy student
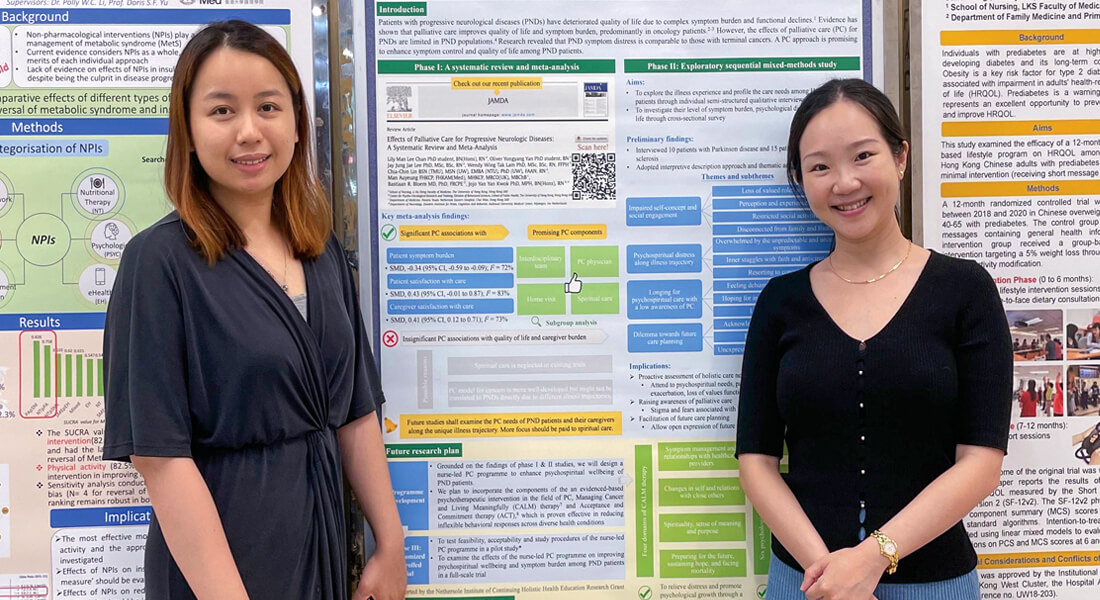
The U21 Health Sciences Nursing and Midwifery Group Research Postgraduate Symposium 2024 was a valuable platform for postgraduate students to disseminate research findings and exchange knowledge worldwide. I was honoured to present my PhD research on palliative care needs for progressive neurological diseases (PNDs) and receive the outstanding presentation award.
My research passion stems from my prior work experience as a nurse in acute hospitals, where care often centres around physical symptoms. Recognising the limitations in psychospiritual care within these settings ignited my unwavering commitment to enhancing psychospiritual support care for patients in the community.
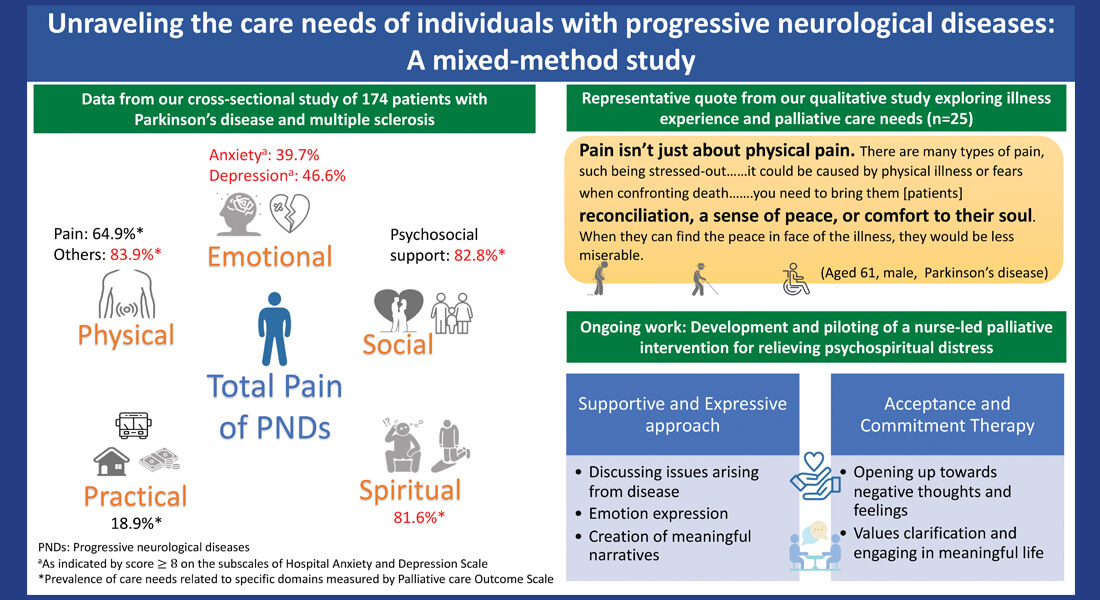
I have been fortunate to embark on my PhD journey with the support of the Hong Kong PhD Fellowship Scheme and the HKU Presidential Scholar Programme. My research endeavours began with a mixed-method study exploring palliative care needs of patients with PNDs, specifically Parkinson’s disease and multiple sclerosis. These conditions not only result in mobility impairments but also bring about a multitude of non-motor symptoms, leading to psychosocial and spiritual distress. However, conventional care for PNDs prioritises motor symptom management.
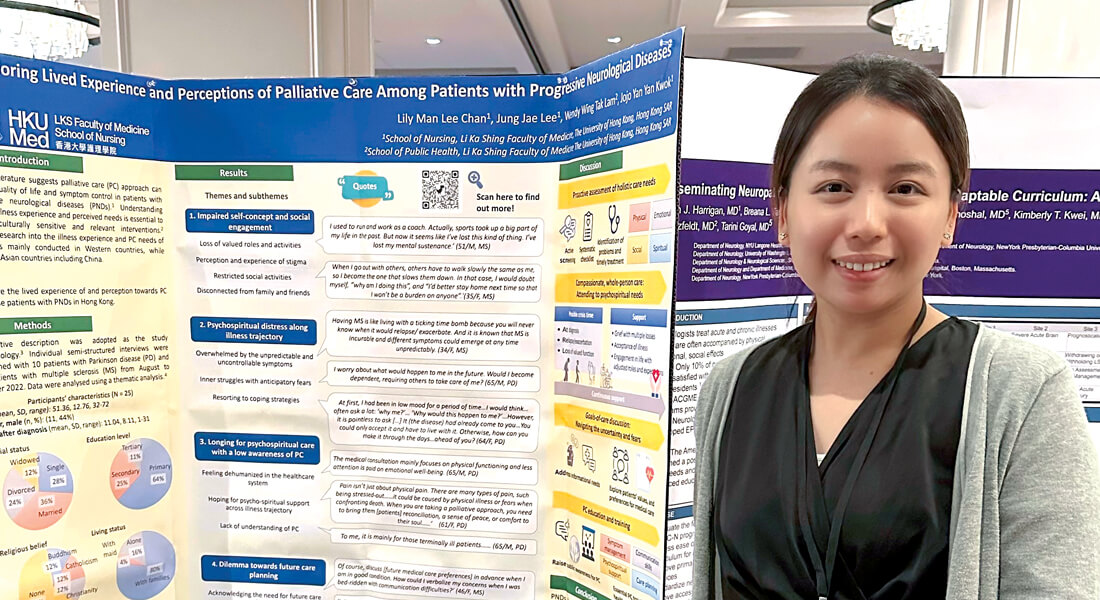
I recently conducted 25 qualitative interviews with PND patients in Hong Kong. It is worth noting that informants expressed significant psychospiritual distress and stressed the need for holistic care that compassionately addresses their symptom burden. A subsequent survey involving 203 patients echoed these interview findings, indicating a diminished quality of life and pronounced palliative care needs. Over 83% of participants reported psychosocial and spiritual needs, comparable in magnitude to their physical needs (86%). A significant proportion exhibited clinically relevant levels of anxiety (39.9%) and depressive symptoms (47.8%).
Palliative care, traditionally implemented in advanced cancer care, is a holistic approach that aims to optimise patients’ quality of life by addressing physical, psychosocial, and spiritual needs. Despite the European Academy of Neurology guideline advocating palliative care for PNDs, empirical evidence specifically for these conditions remains scarce.
To fill the gaps, we initiated a nurse-led, community-based palliative programme, namely “Cultivating Acceptance and Living Meaningfully with Progressive Neurological Diseases” (CALM-Neuro), to promote acceptance and value-based living. The CALM-Neuro intervention aims to address psychospiritual concerns through a supportive and expressive approach and incorporate evidence-based psychological techniques including mindfulness and acceptance and commitment-based components. We are grateful to have received funding from the Health and Medical Research Fund, Health Bureau and the Nethersole Institute of Continuing Holistic Health Education to examine the feasibility and preliminary effects of CALM-Neuro in the realm of palliative care. Preliminary findings show promise in improving psychospiritual outcomes. Participants perceived CALM-Neuro as a unique opportunity to process their experience of living with PNDs and discuss their psychospiritual concerns. We look forward to sharing the results in the near future.
As a PhD student, I advocate for a palliative care approach that addresses the unique needs of patients with PNDs. I am committed to developing evidence-based nursing practices that alleviate symptom burden and empower patients to navigate psychospiritual challenges throughout their illness trajectory. I believe nurses, equipped with clinical competency and appropriate mental health training, are uniquely positioned to identify at-risk individuals and deliver brief yet impactful interventions. I am committed to further research that integrates psycho-behavioral approaches into palliative care for PNDs.
Back